E. cuniculi Series
series by
Megan Schommer, DVM.
Dr. Schommer shares high-quality, evidence-based information about exotic companion mammals on her personal Faceboook blog page. She is a member of the Minnesota Veterinary Medical Association (MVMA), American Veterinary Medical Association (AVMA), and the Association of Exotic Mammal Veterinarians (AEMV).
Below is her multi-part series on E. cuniculi (EC), reposted here with her direct permission.
Basic Info
Part 1 posted on: October 11, 2020
Let's start with a few definitions and basic information about the disease so that we're all on the same page.
E. cuniculi (EC) is an obligate intracellular parasite from the class Microsporidia, which for the moment is considered a form of fungus. EC can infect all mammalian species, including humans, although rabbits, guinea pigs, and mice are considered the primary reservoirs. EC doesn't typically cause disease in humans unless they are immunocompromised, but this is important to keep in mind since that means infected rabbits who are shedding the organism have zoonotic potential to immunocompromised/immunosuppressed owners.
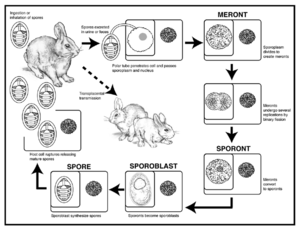
Animals become exposed to EC via vertical transmission (being infected in utero) or via ingestion or inhalation of spores that are excreted in the urine of an infected animal. Upon exposure, the infectious spores first infect organs with high blood flow (kidneys, liver, and lungs), and later move to the nervous system. As the organisms multiply within thick-walled spores, the spores eventually rupture, causing an inflammatory response in the surrounding tissues. It is suspected that the inflammatory response is more responsible for the signs of disease rather than the organism itself. The most common site affected by disease are the ocular, renal, and neurologic tissues. Infected rabbits shed spores in their urine beginning about 1 month after infection, and shed spores in high quantities for about 2.5 months. Rabbits can continue to shed intermittent, low quantities of spores as long as they remain infected. Eventually, the rabbit's body is able to wall off these organisms and the inflammatory response subsides even though the organisms are still present within the tissues (Quesenberry et al. calls this a "balanced host/parasite relationship"). The EC organisms continue to remain viable. Stress, disease, or anything that causes immunosuppression can disrupt this balance and allow the parasite to suddenly start causing signs of disease even if it was many years after the initial infection.
Based on serology (evidence of antibodies against EC), healthy rabbit populations can have upwards of 75% of individuals show exposure to EC. EC organisms are ubiquitous (found in the environment, soil, etc), and so exposure is very common. This does not mean that 75% of rabbits will develop disease associated with their exposure to the organism. I'll get more specific about serologic testing and the challenges associated with diagnosing EC infections in rabbits in a later post.
Resources used:
- Carolyn Cray, Madisen P. Liebl, Kristopher Arheart, Roman Peschke, Frank Künzel, Anja Joachim, Comparison of enzyme-linked immunosorbent assay and immunofluorescence test for determination of anti-Encephalitozoon cuniculi antibodies in sera from rabbits with different clinical and histopathological presentations, Journal of Exotic Pet Medicine, Volume 32, 2020, Pages 39-42, ISSN 1557-5063, https://doi.org/10.1053/j.jepm.2019.11.003.
- Peter G. Fisher, Frank Künzel, Helena Rylander, 18 - Neurologic and Musculoskeletal Diseases, Editor(s): Katherine E. Quesenberry, Connie J. Orcutt, Christoph Mans, James W. Carpenter, Ferrets, Rabbits, and Rodents (Fourth Edition), W.B. Saunders, 2020, Pages 233-249, ISBN 9780323484350, https://doi.org/10.1016/B978-0-323-48435-0.00018-6.
Clinical Signs
Part 2 posted on: October 22, 2020
This post is the second in my series on E. cuniculi, and today we'll be reviewing the clinical signs associated with E. cuniculi infection. It's important to remember that not all rabbits who are exposed to E. cuniculi become infected, and not all infected rabbits will develop symptoms.
There are three main organ systems that are targeted by E. cuniculi: the eyes (specifically the lens of the eye), the kidneys, and the brain. We'll take these one at a time.
Ocular manifestations: Rabbits who develop eye disease due to E. cuniculi were exposed in utero. Cataracts can develop in one or both lenses, as well as leakage from or rupture of the lens. "Phacoclastic uveitis" is the most severe end stage of ocular E. cuniculi, in which the lens ruptures and causes severe inflammation within the eye. Rabbits who experience this can develop pain, glaucoma, and blindness unless the lens material is removed through a specialty procedure called phacoemulsification. The procedure needs to be performed early on in the course of uveitis to have the best chance of restoring comfort and keeping the eye visual. Without quick treatment, affected eyes become blind and surgical removal should be considered as these eyes are at risk of developing glaucoma. Rabbits with ocular lesions of E. cuniculi should be diligently monitored for the other types of diseases associated with E. cuniculi infection since the organism is often present throughout the body.
Kidneys: E. cuniculi in the kidneys causes an inflammatory nephritis, followed by fibrosis. In some animal, this doesn't cause enough damage to have any long-term effects, but if enough damage occurs, then the kidneys lose their ability to concentrate urine and sometimes their ability to filter toxins. The most common clinical signs of renal disease in rabbits include polyuria/polydipsia (oftentimes with secondary urine scald from urinary incontinence), weight loss, and general signs of malaise (unkempt haircoat, poor muscling, lethargy).
Brain: Signs of central nervous system dysfunction are the most well-known manifestation of E. cuniculi. Common clinical signs reported to be associated with E. cuniculi infection include vestibular disease (head tilt, torticollis, nystagmus), seizures, and hindlimb paralysis or paresis (although there is at least some debate about how commonly paralysis/paresis are due to E. cuniculi- Quesenberry states that one of the authors (Dr. Frank Kunzel) "believes that these neurologic signs are often falsely attributed to the organism"). Episodes of vestibular disease often follow stressful events or develop secondary to some other systemic illness, which supports the theory that immunosuppression allows E. cuniculi to come out of dormancy and start reproducing, causing inflammation which induces clinical signs. Important differentials for head tilt in rabbits include otitis interna, neoplasia, and dental disease. It's easy to see a head tilt and immediately blame E. cuniculi, but of course we see head tilts develop in many other species that don't have E. cuniculi infections, so don't forget to include other causes on your differential list. Quesenberry et al. suggests that unilateral facial dysfunction or spasm are more likely to be seen with otitis interna than E. cuniculi.
A recent study of three large rabbit farms in Egypt found that out of 16,400 rabbits, a whopping 13,242 rabbits had clinical signs suggestive of E. cuniculi (including head tilt/vestibular signs, cataracts, phacoclastic uveitis, and signs of PU/PD such as urine scald). 81.5% of these rabbits had neurologic signs, 10.5% had ocular lesions (cataracts, phacoclastic uveitis), and 2.7% had signs of pulyuria. I'll admit that this study is complex and I don't quite understand how many of the rabbits were confirmed to have E. cuniculi on necropsy, but if anyone wants to dig into the details, full text is available at https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7036226/.
Resources used:
- Peter G. Fisher, Frank Künzel, Helena Rylander, 18 - Neurologic and Musculoskeletal Diseases, Editor(s): Katherine E. Quesenberry, Connie J. Orcutt, Christoph Mans, James W. Carpenter, Ferrets, Rabbits, and Rodents (Fourth Edition), W.B. Saunders, 2020, Pages 233-249, ISBN 9780323484350, https://doi.org/10.1016/B978-0-323-48435-0.00018-6.
- Anna L. Meredith, Jenna Richardson, Neurological Diseases of Rabbits and Rodents, Journal of Exotic Pet Medicine, Volume 24, Issue 1, 2015, Pages 21-33, ISSN 1557-5063, https://doi.org/10.1053/j.jepm.2014.12.007.
- Morsy EA, Salem HM, Khattab MS, Hamza DA, Abuowarda MM. Encephalitozoon cuniculi infection in farmed rabbits in Egypt. Acta Vet Scand. 2020;62(1):11. Published 2020 Feb 22. doi:10.1186/s13028-020-0509-6.https://dx.doi.org/10.1186%2Fs13028-020-0509-6
Diagnosis
Part 3 posted on: October 29, 2020
So, you think your rabbit patient might have E. cuniculi. She's developed an acute head tilt, or has phacoclastic uveitis, or has primary renal azotemia. You'd like to do some testing to see if E. cuniculi might be the cause. What's the right diagnostic test to run? This is a bit of a loaded question because, unfortunately, the majority of the time we cannot make a definitive diagnosis. Rabbits can be EXPOSED to E. cuniculi, but not infected. Rabbits can be INFECTED with E. cuniculi, but not develop disease. And rabbits can have syndromes often associated with E. cuniculi, like those listed above, and have some other disease process occurring (even if they also happen to be infected by E. cuniculi).
The only way to definitively say that a rabbit has been infected by E. cuniculi is to find the organism within the tissues on a biopsy. This is rarely something that we manage to do on a live rabbit, since it would require collecting tissue from the eye, brain, or kidney (although, if a rabbit needs an eye removed due to phacoclastic uveitis, that's a great opportunity to submit tissues for biopsy). Early on in the course of disease, E. cuniculi spores are shed in the urine, but this only happens intermittently, and the shedding period can occur long before a rabbit shows any signs of disease (the lab at UF-Miami tried examining urine samples alongside blood samples to see if screening for urine spores was helpful, but unfortunately urine testing didn't provide any useful information).
Titer Testing
So, what we are left with is an imperfect antemortem tool called titer testing. Titer testing involves collecting a blood sample and measuring the numbers of antibodies created against the E. cuniculi organism. Different types of antibodies respond to infection at different times. IgM antibodies tend to rise earlier on in the course of infection, and IgG antibodies tend to develop later. A paper by Cray et al (2020) references a study of experimentally-infected rabbits that developed IgM titers about a week post-infection and showed that they maintained a detectable IgM titer at 18 weeks post-infection; a second study referenced showed that IgM titers started to decline around 35 days post-infection. This is a clue that rabbits with high or rising paired IgM titers most likely have an acute infection or reactivation of a chronic infection.
The University of Miami is generally considered to be the go-to lab for sending E. cuniculi labwork, as Dr. Carolyn Cray in the Avian and Exotics Lab has special interest in researching E. cuniculi. Some labs will only provide you with a "positive" or "negative" result, but this information is less helpful than getting a quantitative titer, which tells you not just that a rabbit has made antibodies but also how many. There is some nuance involved in interpreting what a low titer means vs a high titer (i.e. having a high titer doesn't necessarily mean a rabbit has more severe disease), but having titer levels above a certain threshold is more likely to indicate active disease rather than historic exposure. Currently, the University of Miami recommends checking an IgM and IgG titer in addition to a level called C reactive protein (CRP), which is a protein that becomes quickly elevated in the face of inflammation. This is the most reliable panel of tests that we currently have for evaluating a rabbit for E. cuniculi infection. Abnormal results in all three of these values are quite indicative of an active E. cuniculi infection.
The major diagnostic challenge comes when only one or two of these three values are abnormal. Many, many clinically normal rabbits have positive titers and never show signs of disease (upwards of 50% of healthy rabbit populations can have positive titers). The most helpful result is finding a negative titer, as that is a pretty reliable indicator that you can cross E. cuniculi off your list of possible causes. The other helpful result is a high IgM titer, high IgG titer, and elevated CRP in a patient showing signs consistent with E. cuniculi infection- that all information helps you know that proceeding with treatment for E. cuniculi is the best next step. In patients who have suspicious clinical signs, but have a low IgM or IgG titer, or have a high IgG/low IgM, or low IgM/high IgG, high titers but low CRP, etc etc... all becomes much more confusing to interpret.
If you've run your E. cuniculi panel on a rabbit patient showing suspect signs, and you've also done good baseline labs to screen for concurrent issues that might be causing disease, you might find yourself in this conundrum where you still don't have a clear answer. Unfortunately, this is the nature of the disease at the moment. Dr. Cray is a wonderful resource and may be able to give you guidance about how to interpret your panel. And if you have an interesting E. cuniculi case to share, she is constantly researching this disease and may be interested in hearing about your experience. You can find her contact information, plus a great breakdown of interpretation of titers, at http://cpl.med.miami.edu/avian-and-wildlife/ecun/. I hope that this is helpful, although it is probably clear as mud. Sorry, all. Next up: treatment options.
Resources used:
- Carolyn Cray, Madisen P. Liebl, Kristopher Arheart, Roman Peschke, Frank Künzel, Anja Joachim, Comparison of enzyme-linked immunosorbent assay and immunofluorescence test for determination of anti-Encephalitozoon cuniculi antibodies in sera from rabbits with different clinical and histopathological presentations, Journal of Exotic Pet Medicine, Volume 32, 2020, Pages 39-42, ISSN 1557-5063, https://doi.org/10.1053/j.jepm.2019.11.003. (https://www.sciencedirect.com/science/article/abs/pii/S1557506319301892)
- Peter G. Fisher, Frank Künzel, Helena Rylander, 18 - Neurologic and Musculoskeletal Diseases, Editor(s): Katherine E. Quesenberry, Connie J. Orcutt, Christoph Mans, James W. Carpenter, Ferrets, Rabbits, and Rodents (Fourth Edition), W.B. Saunders, 2020, Pages 233-249, ISBN 9780323484350, https://doi.org/10.1016/B978-0-323-48435-0.00018-6.
- F.M Harcourt-Brown, Encephalitozoon cuniculi infection in rabbits, Seminars in Avian and Exotic Pet Medicine, Volume 13, Issue 2, 2004, Pages 86-93, ISSN 1055-937X, https://doi.org/10.1053/j.saep.2004.01.004. (https://www.sciencedirect.com/science/article/abs/pii/S1055937X04000064)
Treatment
Part 4 posted on: November 29, 2020
This post has been a tricky one to write because, unfortunately, there isn't a whole lot of evidence-based information regarding the treatment of E. cuniculi. I'll do my best to present what we know based on research, and then what most of us actually do in practice.
The short version: most veterinarians treat E. cuniculi signs with a medication called fenbendazole (Panacur), administered at a dose of 20 mg/kg once daily for 28 days.
The long version: As best I can determine, the above treatment regimen can be traced back to a single study published in 2001 by Suter et al. This was a small study of 17 client-owned rabbits that had E. cuniculi antibody titers of >1:640. 8 of these rabbits were fed medicated pellets for four weeks which were estimated to have administered about 20 mg/kg/day of fenbendazole over the four week period. 9 rabbits were not treated. 6 of the 8 treated rabbits died of causes unrelated to E. cuniculi. 2 of the 8 treated rabbits were euthanized following the four week treatment period due to persistent neurologic signs. Of the untreated rabbits, 4 out of 9 died of neurologic signs consistent with E. cuniculi infection. The remaining 5 died of disease not related to E. cuniculi. Post mortem, the authors were able to isolate E. cuniculi from 7 out of 9 of the untreated rabbits, but 0 out of the 8 treated rabbits.
Suter et al. concluded: "The fact that the treatment eliminated tissue parasite stages was shown by the reduction of tissue spores to below the detection threshold in all the treated rabbits."
As with most studies in veterinary medicine, this is an embarrassingly small sample size on which to base our entire treatment protocol, but here we are. And, while this study demonstrated that the treated rabbits seemed to have the parasite suppressed to non-detectible levels in their brains, 2 of the 8 treated rabbits still were ill enough with neurologic signs to warrant euthanasia, giving support to the theory that the inflammation from the parasites may be just as disease-causing as the presence of the parasites themselves.
Fenbendazole is an antiparasitic drug in the benzimidazole class. A 1995 study by Franzen et al. showed that several benzimidazoles, including albenazole, thiabendazole, and oxibendazole had in vitro efficacy against E. cuniculi in rabbit kidney cells. Kotler and Orenstein (1999) found fenbendazole to also have in vitro efficacy against E. cuniculi.
Edited to add one more resource:
I don't have access to the original study referenced here (Jessica Sieg, Jutta Hein, Ariane Jass, Carola Sauter-Louis, Katrin Hartmann, Andrea Fischer, Clinical evaluation of therapeutic success in rabbits with suspected encephalitozoonosis, Veterinary Parasitology, Volume 187, Issues 1–2, 2012, Pages 328-332, ISSN 0304-4017, https://doi.org/10.1016/j.vetpar.2011.12.014 (http://www.sciencedirect.com/.../pii/S0304401711008521 ) ). I do have access to a 2014 paper that references the Sieg study from Latney et al. (2014), and they summarize the Sieg findings here: "A recent study, conducted by Sieg et al, has evaluated the clinical efficacy of fenbendazole, oxytetracycline, and steroid therapy. There was no significant difference in the long-term or short-term survival or in neurologic sign reduction in rabbits receiving the following treatment combinations: oxytetracycline + dexamethasone, fenbendazole + dexamethasone, fenbendazole + oxytetracycline + dexamethasone, and oxytetracycline alone. Dexamethasone did not appear to have a therapeutic effect. Survival analysis performed for those rabbits that received fenbendazole demonstrated that they were 1.6 times more likely to survive until day 10 compared with rabbits that did not receive fenbendazole in their treatment protocol. After day 10, there was no consistency in the efficacy of fenbendazole. This demonstrates the need for more controlled studies that histologically demonstrate spore reduction based on the treatment protocol."
This is pretty much the extent of the research about treatments for E. cuniculi. Quesenberry says it pretty well: "In the absence of controlled studies, assessing the efficacy of therapeutic agents against E. cuniculi is difficult because latent infections occur, and some clinical cases may improve spontaneously without treatment, presumably because of the host’s immune response... With most of the suggested drugs, susceptibility of the pathogen has not been assessed in clinical settings."
Ugh. Lame.
This lack of clear evidence of clinical efficacy is on its own frustrating, but if the treatment fell into the category of "might help/can't hurt", at least it gives us something to reach for as a possible treatment option. But unfortunately, there are multiple documented cases of benzimidazole toxicity in rabbits. Graham et al. reported 13 cases of toxicity in rabbits related to benzimidazole administration (12 of the 13 rabbits died). Toxicity primarily manifests as pancytopenia (lack of red blood cells, white blood cells, and platelets) due to bone marrow suppression. This leads to immunosuppression and secondary sepsis, and/or clotting abnormalities- both of which are often fatal. In this study, the dosages used were higher than the recommended dosage in 7 of the 13 rabbits. "It may be prudent to have baseline blood work on rabbits before, during, and after the initiation of benzimidazole treatment. If anemia, leukopenia, or thrombocytopenia is noted after starting benzimidazole treatment, immediate discontinuation of drugs may be helpful to slow or stop progression of toxicosis. As the first rabbit deaths were reported during the initial 14 days of benzimidazole treatment, it may be advisable to consider weekly CBC during therapy."
So, we have a therapy that may or may not actually help in the clinical setting, but that we definitely know can cause significant bone marrow toxicity and can lead to death. Disappointing, to say the least. My hope is that, because E. cuniculi presents a zoonotic risk to immunocompromised humans, there will at some point be enough interest in finding effective treatments and preventative measures that it will spill over into research that benefits our companion rabbits.
I'll follow up soon with other treatment options that can help supportively, even if not specifically, and then finish with a post about possible preventative measures. Stay tuned!
Resources used:
- Peter G. Fisher, Frank Künzel, Helena Rylander, 18 - Neurologic and Musculoskeletal Diseases, Editor(s): Katherine E. Quesenberry, Connie J. Orcutt, Christoph Mans, James W. Carpenter, Ferrets, Rabbits, and Rodents (Fourth Edition), W.B. Saunders, 2020, Pages 233-249, ISBN 9780323484350, https://doi.org/10.1016/B978-0-323-48435-0.00018-6
- Franssen, F. F., Lumeij, J. T., & van Knapen, F. (1995). Susceptibility of Encephalitozoon cuniculi to several drugs in vitro. Antimicrobial agents and chemotherapy, 39(6), 1265–1268. https://doi.org/10.1128/aac.39.6.1265
- Jennifer E. Graham, Michael M. Garner, Drury R. Reavill, Benzimidazole Toxicosis in Rabbits: 13 Cases (2003 to 2011), Journal of Exotic Pet Medicine, Volume 23, Issue 2, 2014, Pages 188-195, ISSN 1557-5063, https://doi.org/10.1053/j.jepm.2014.02.012.(https://www.sciencedirect.com/science/article/abs/pii/S1557506314000469)
- Latney, L. V., Bradley, C. W., & Wyre, N. R. (2014). Encephalitozoon cuniculi in pet rabbits: diagnosis and optimal management. Veterinary medicine (Auckland, N.Z.), 5, 169–180. https://doi.org/10.2147/VMRR.S49842
- Ritzman, Tracey K. 2015. "Encephalitozoon cuniculi in Rabbits: What Do We Know About Treatment Options?" ABVP Proceedings.
- Suter C, Müller-Doblies UU, Hatt JM, Deplazes P. Prevention and treatment of Encephalitozoon cuniculi infection in rabbits with fenbendazole. Vet Rec. 2001 Apr 14;148(15):478-80. doi: 10.1136/vr.148.15.478. PMID: 11334074.
Supportive Care
Part 5 posted on: December 30, 2020
We established in the last post that there is a dearth of evidence for specific treatment of E. cuniculi in rabbits (at least in the setting in which most of us are treating rabbits- client-owned, naturally-infected rabbits, not laboratory or experimentally-infected rabbits). There are other treatments that are often utilized supportively for suspect E. cuniculi patients that also may or may not be helpful, and evidence-based studies are basically absent. Acknowledging that the plural of anecdote is not data, here are the other things that are sometimes utilized:
1) Nutritional and Fluid Support. As with any condition in rabbits that causes pain, fear, or stress, acute onset of signs associated with E. cuniculi can induce bouts of GI stasis. Any loss of appetite or decrease in defecation needs to be addressed promptly. Rabbits with head tilts or ataxia might struggle to get to their food bowls, and rabbits with kidney disease might not eat well due to azotemia. Support feeding with products like Critical Care or Emeraid Herbivore can help prevent stasis until rabbits start eating on their own. Subcutaneous or IV fluid therapy may be needed if rabbits are unable to safely access a water bowl or water bottle.
NSAID
2) Anti-inflammatory Medications. Cell rupture due to E. cuniculi causes inflammation to surrounding tissues, and it is theorized that much of the clinical disease associated with E. cuniculi infections is due to the inflammatory reaction rather than the organism itself. Meloxicam (Metacam) is the most common anti-inflammatory utilized. Glucocorticoids (steroids) have been shown in at least one study to have no beneficial effect in the treatment of rabbits with E. cuniculi, and we know that rabbits are relatively susceptible to the immunosuppressive effects of steroids which, at least in theory, could make an E. cuniculi infection worse. Baseline labwork should ideally be performed in case the patient has kidney disease associated with E. cuniculi, which could make NSAID use contraindicated.
3) Anti-nausea Medications. Vestibular disease can make animals profoundly nauseated, and anti-motion sickness medications such as meclizine (Bonine) are commonly prescribed to help reduce nausea. We know that rabbits cannot vomit, but I don't see any reason why they couldn't become nauseated. Quesenberry et al. disagrees, writing "Also, vestibular dysfunction in rabbits is most probably not associated with nausea, because they usually will eat spontaneously, even with severe torticollis. Therefore, in contrast to dogs and cats, antiemetic drugs are not indicated in rabbits with vestibular disease."
4) Sedation. Rabbits who are acutely affected by vestibular disease can be distressed, especially if they are rolling, and a little bit of midazolam can go a long way.
5) B Vitamins? I see this mentioned in the literature occasionally as part of a treatment plan for E. cuniculi or any other condition that might prevent rabbits from ingesting their cecotropes. There's no specific evidence supporting the use of B vitamins, but since they are water-soluble, you can't really overdose B vitamins. Can't hurt, might help? This one is not evidence-based as far as I can tell.
6) Physiotherapy. Encouraging hopping, at least once rabbits are "with it" enough to get themselves moving, can help with re-equilibration following the onset of vestibular disease. We know in human medicine that the earlier one starts moving following a brain injury, the better. It's reasonable to think the same might be true for rabbits. http://www.disabledrabbits.com/physical-therapy.html has some really nice videos and suggestions for ways to improve mobility following a vestibular episode! Physical therapy is probably more important than any of the medications that we utilize.
7) Acupuncture. Any nervous system dysfunction has the potential to improve with acupuncture, although I've not attempted to dig into acupuncture-specific literature to see if anyone has developed protocols specifically for vestibular disease in rabbits. Please let me know if you are aware of any and I will add it to a resource list!
8) Hygiene. Especially for rabbits with kidney disease due to E. cuniculi, nursing care to keep them clean and dry is very important. Polyuria leads to urinary leakage for many rabbits, with secondary urine scald and skin infections. Frequent bedding changes to keep them dry is essential. Long-haired rabbits might benefit from keeping the hair on their ventrum trimmed short. Rabbits who are acutely vestibular may struggle to get to their cecotropes, which can lead to messy bottoms (note that most bunnies will eat their cecotropes if they are brought to their faces... gross, I know, but those little nutrient-dense packets are so important!).
9) Diagnostics. Keep searching for any other underlying causes! As we've delved into this topic, it's become clear how messy the diagnosis of disease due to E. cuniculi can be. If rabbits are failing to respond to treatment, it may be because we don't actually have a great protocol for treating E. cuniculi, or it might be that E. cuniculi is sometimes a diagnosis of exclusion, and we really need to be thorough about looking for other causes of disease (i.e. otitis interna, neoplasia, dental disease) before we jump to E. cuniculi. Don't forget to do your due diligence. Get your minimum database (CBC, chemistry, UA, E. cuniculi titers, radiographs- especially skull radiographs) and be sure you aren't missing another disease process- especially if your patient is failing to improve. We do our patients a disservice if we don't make a full differential list.
I'll plan to do one last post about prevention soon. Thanks for sticking with this series!
Prevention
Part 6 posted on: February 22, 2021
Hello everyone! Thank you for your patience awaiting the final installment of my series about E. cuniculi. It's been a busy couple of months at work so this has been on the back burner, but I want to wrap this series up with some information about prevention of E. cuniculi in companion rabbits.
The evidence-based research on preventing E. cuniculi in a population is, unfortunately, scarce. Most of the literature focuses on research populations, which can be kept pathogen-free with strict biosecurity protocols. This isn't the case with companion rabbits, who might have access to backyards, "hoppy hours", or bonding sessions with new buddies. I have read about some practitioners who advise using Panacur (fenbendazole) once weekly for life, or for a month following introduction of a new rabbit, or one month every year to keep the reproduction of E. cuniculi at bay. Unfortunately, there is no evidence to support any of these protocols. We have to keep in mind that some rabbits will develop bone marrow suppression from fenbendazole, and if there is no actual evidence that the use of this drug could prevent the replication or shedding of this organism, is it worth risking a known (and potentially fatal) side effect?
I think, if I had to come up with a recommended protocol to try to prevent E. cuniculi, I would recommend that people at least know the status of their own rabbits' exposure to E. cuniculi. If your rabbit has no antibodies, and you intend to bond them to another rabbit, it would be helpful to know if the new rabbit has antibodies (and thus could potentially be shedding spores during periods of stress, such as times when a rabbit is introduced into a new home). If your rabbit has antibodies, it would be nice to know if a rabbit you are introducing doesn't, because you might be extra vigilant about watching for neurologic signs or signs of kidney disease in your new rabbit in the month or two after introducing them.
Knowing your rabbit has been exposed may affect how safe you feel having your bun interact with other rabbits. Do I think that everyone should titer test their rabbits prior to having them interact at "hoppy hours", introducing a newly-adopted bun, or be shown at rabbit shows? Gosh... I don't know. We know that rabbits can get exposed to E. cuniculi from spores shed into the environment, so even if a rabbit has a negative titer today, it might have a positive titer in two months, even with no direct exposure to other rabbits in the interim. I hope this series has been helpful! I, like most people, wish we knew a lot more about this disease. Please let me know if there are specific questions you have that I didn't address!
See also