Gastrointestinal stasis
Gastrointestinal stasis, GI stasis, GI hypomotility or ileus is a serious condition that requires immediate attention. The condition occurs when the gut stops moving, is blocked, or is full of gas.
Symptoms

- Loss of appetite (anorexia) or changes in eating habits. A good way to test this is to offer fresh herbs or a favorite treat.
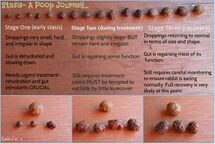
- Small to no stool, loose or mucous covered stool or diarrhea.
- Sitting in a hunched position or pressing stomach against the floor.

- Loud tooth grinding which is an indication of pain. This is different than the "tooth purr" that indicates pleasure or contentment.
- Loud GI sounds or complete silence in the stomach. You can use a stethoscope or listen with your ear pressed against the stomach.
Causes
- Stress. Examples of stressful events include changes in housing, introduction of new rabbits or other pets, recent illness, trauma, or surgery.[1]
- Pain from an underlying condition (e.g. gas, dental problems, upper respiratory tract disease, neurological disorders, gastric ulcers, or hepatic, renal, or urinary tract disorders).[1] Rabbits in signs of pain are reluctant to move, appear less social, may grind their teeth, may dig or scratch, and sit in a hunched position.
- Dehydration.
- Lack of dietary fiber. Rabbits whose regular diet consists primarily of pelleted feeds are at higher risk of developing GI stasis as the pellets are usually high in calories (high in digestible carbohydrates), low in fiber, high in protein, and highly digestible.[1] Similarly, rabbits routinely fed large amounts of high-simple carbohydrate, high-fat treats such as nuts, seeds, baked goods, and fruits are also predisposed to GI stasis.[1] Acute episodes of GI stasis and dysbiosis are common following ingestion of a large volume of these treats.[1]
- Intestinal blockage. This usually leads to an episode of acute gastrointestinal dilation instead.
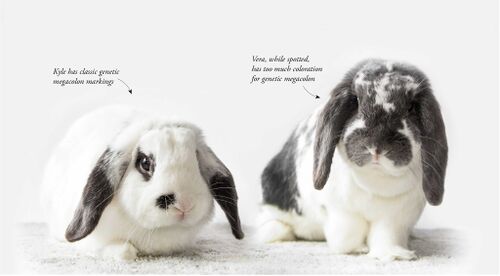
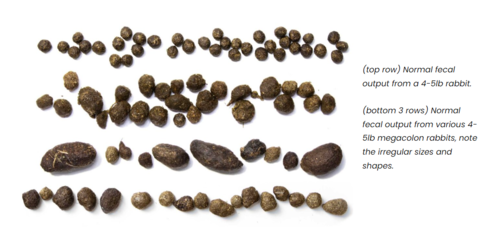
- Genetic condition. Rabbits that are mostly white can have a genetic condition called megacolon.
Diagnosis
Gastrointestinal stasis can be usually diagnosed as non-obstructive or obstructive ileus.

| Non-obstructive | Obstructive | |
|---|---|---|
| Clinical Signs |
|
|
| Radiographic findings |
|
|
From Keeble, E & Meredith, A. (2006). Rabbit medicine & surgery: Self-assessment color review.
When palpating an affected rabbit's stomach, the stomach usually feels firm and doughy and remains pitted on compression.[1]
Rabbits with GI stasis have few or no gut sounds (borborygmi).[1] Rabbits under normal conditions should have at least 3-4 good sounds per minute.[2]
Treatment
You should seek immediate veterinary assistance if your rabbit has not eaten or passed stools in the past 12 hours or is exhibiting other symptoms of GI stasis. Your vet will provide proper treatment and care. If left untreated, GI stasis can be fatal in 48 hours, especially if it is a secondary symptom to another urgent condition like liver lobe torsion or gastric ulceration.
The key principles in the treatment of GI stasis are the following:[1] [3]
- rehydrating the rabbit and stomach contents
- restoring appetite
- correcting electrolyte imbalances
- stimulating gastric emptying
- promoting normal gastrointestinal motility
- softening and lubricating impacted food and hair
- alleviating pain
- providing nutrition
- treating any underlying disorders
Rabbits should receive fluids either intravenous, intraosseous, or subcutaneously, depending on the severity of dehydration. Stomach contents can also be rehydrated by assisted feeding with a syringe.[3] A popular commercial product for this purpose includes Oxbow Critical Care for Herbivores. Other alternative commercial brands can be found at First aid for rabbits#Syringe feeding. If these formulas are not available, blended pellets soaked with water or an oral electrolyte solution can be used.[3] Pureed vegetables or baby foods are also an option, but these foods are not sufficiently high in fiber.[1] Force feeding these formulas can help prevent hepatic lipidosis, which can develop quickly in a rabbit with a negative energy balance.[3]
Rabbits with GI stasis usually have mild to severe gut pain, especially if the intestines are distended with gas, and will not eat until the pain is alleviated.[3] Appropriate drugs include buprenorphine and a nonsteroidal anti-inflammatory drug (NSAID) such as meloxicam or carprofen.
GI prokinetics are commonly used for GI stasis treatments. The use of intestinal prokinetic agents is somewhat controversial, but anecdotal evidence suggests that they may be beneficial.[3]
- Cisapride is readily absorbed from the GI tract and promotes gastric emptying, increases gastrointestinal and colonic motility.[3][1] It acts on both the foregut and hindgut and does not increase gastric acid secretion.[1] The effects last for 4 to 10 hours and stimulates appetite, especially for fibrous foods such as grass or hay.[1] Cisapride is contraindicated in patients with mechanical gastrointestinal obstruction, haemorrhage or perforation and can have fatal interactions in rabbits with antifungal drugs such as ketoconazole, itraconazole or miconazole by causing fatal cardiac arrhythmias.[1]
- Metoclopramide promotes gastric emptying and increases gastrointestinal motility in rabbits, and it does not affect the hindgut or gastric, pancreatic or biliary secretion.[1] Like cisapride, metoclopramide is contraindicated in rabbits with a GI obstruction.[1]
- Maropitant citrate (Cerenia) is a newer medication commonly used as an anti-nausea in dogs that has been used for rabbits in stasis. While its anti-nausea properties are not useful for rabbits since they cannot vomit, users have seen positive results as a prokinetic and to relieve gut pain and soothe the GI tract.[4]
If evidence of dysbiosis is present, antibiotics such as enrofloxacin and trimethoprim-sulfamethoxazole may be needed. If enterotoxemia is suspected, metronidazole should be administered.
Liquid paraffin can be used to soften and lubricate impacted stomach or cecal contents and should be administered with care (preferably mixed with food) as it is easily aspirated.[1]:321
Care should be used when protein-digesting enzymes such as pineapple for bromelain and papain. They can be very irritating to the oral and gastric mucus.[3] The risk of gastic ulceration is increased in anorexic rabbits, and use of these enzymes can make this a bigger problem.[3] Additionally, the recommendation that these products can dissolve hair is false, and the success of pineapple juice as a remedy may be due to the introduction of liquid rather than the enzyme.[1]
Petroleum laxatives such as Petromalt and Laxatone are of questionable value, but some veterinarians report anecdotal improvement as a preventative medication.[3]
In the very rare case, a dehydrated mass of material in the stomach can form a solid immovable mass and surgical intervention may be necessary. Prognosis for a successful outcome is greatly reduced as anesthesia, pain, stress, and manipulation of the intestinal tract all exacerbate GI stasis, and complications of hepatic lipidosis are a common cause of death in these rabbits.[3] Every hour counts.
At-home treatment
For at-home initial treatment when you first notice symptoms, you can do the following:
- Surround your rabbit with favorite foods. Good choices include vegetables (e.g. cilantro, parsley, and lettuce), their regular pellets, favorite hay-based treats, and alfalfa hay. You can offer a small piece of sweet treats like fruit and carrots, but try to limit the amount of sugar when your rabbit is in gastrointestinal distress.
- Check if your rabbit is losing blood and becoming anemic. This is more to rule out more serious health issues that may make it difficult to keep your rabbit stable throughout the night. You can check their gums or flip over their eyelid to check their mucusa is a shade of pink. If the mucusa looks white, grey, or mauve, then your rabbit is in more dangerous shape, and you should seek any kind of emergency medical help as soon as possible.
- Check the temperature of your rabbit rectally. Normal rectal rabbit temperature should be 101-104°F (38.3-40°C).
 A rabbit buried in blankets with some vegetables in front of her face while she was lethargic from an extremely low body temperature (97°F) during a stasis episode.
A rabbit buried in blankets with some vegetables in front of her face while she was lethargic from an extremely low body temperature (97°F) during a stasis episode.A temperature below 100°F means the rabbit is starting to go into or is already in shock. Rabbits will be very lethargic with decreased responsiveness to stimuli. If you do not have a thermometer on hand, if your rabbit is already lethargic and their ear tips and limbs feel cold, they are likely hypothermic. Immediately start warming up your rabbit with heat support. A heating pad, a plastic bottle full of hot water, a microwaved sock full of rice, or a SnuggleSafe disc should be wrapped in a towel to prevent burns. If you do not have any heating accessories, you can microwave a towel or blanket for 30 seconds to temporarily heat it up, or just wrap your rabbit completely in a towel or blanket. Portable hand warmers are also extremely useful under towels and blankets and should be moved around the body every 5-10 minutes to warm them up. Note that rabbits that were hypothermic when taken to the veterinarian for initial stasis treatment have been studied to be 5 times as likely to die or be euthanized compared to rabbits that were of normal body temperature.[5]
A very high temperature above 106°F also needs immediate attention. You can cool down your rabbit by putting the rabbit in a breezy area and carefully wetting down the ears, their main thermoregulatory organ.
- Check the consistency of your bunny's belly. A dehydrated rabbit will feel doughy. A normal rabbit will have the consistency of a balloon. A bloated rabbit will feel like an overfilled balloon. If your rabbit is bloated, please find your nearest emergency veterinary hospital and start treatment promptly for the best chance of recovery.
Try to keep your bunny hydrated to help break up any masses in the stomach. Offer up herbal non-caffeinated teas and cold wet fresh vegetables nearby within easy access if your rabbit does not seem to want to move.
Refrain from force feeding any water directly with a large syringe as liquids are easy for rabbits to aspirate and cause more serious issues. However, if your rabbit is dehydrated and you do not have subcutaneous liquids on hand, giving liquids carefully with a small 1-3cc syringe is okay. Offer 10-20cc of liquids slowly orally.
You can use the skin tent test to check if your rabbit is well hydrated.
- For an acute gas attack, feed 1 to 2 cc of infant simethicone (20 mg/mL suspension) to your rabbit (all sizes) every hour for the first three hours, then every three to eight hours.[6] This product is easily obtainable in the baby sections in a drugstore, pharmacy, or supermarket as a liquid suspension or 125 mg gel capsules. A bunny can safely receive the contents of half a capsule at the rate described above.[6]For a quick list of rabbit-safe simethicone brands around the world with packaging images, please see the Rabbitors article here.
Simethicone has no known drug interactions and is not absorbed through the intestinal lining. It acts only on a mechanical principle: it changes the surface tension of the frothy gas bubbles in the gut, joining them into larger, easier-to-pass bubbles.[6] While this treatment alone will not return function to the intestinal tract, it appears to have no ill effects.[1]
- Making sure that the stomach is not hard with an obstruction, reach under your rabbit's belly and gently massage your rabbit's abdomen to help stimulate the muscle and break up gas bubbles. Pocket vibrators and vibrating toothbrushes are also great for this purpose. Be sure to keep any massage gentle as an aggressive massage can cause torsion, internal bleeding, or rupture organs. Elevating the hindquarters a few inches can also help any gas pass more easily.[6] In addition to the videos below, also check out Massage for rabbits#Belly massages for more resources. If your rabbit is bloated, do not massage your rabbit and proceed to your closest emergency veterinary hospital instead for the best chance of recovery. Massaging with an obstruction can cause their stomach to rupture from the pressure.
- Keep a quiet environment away from predators and barking dogs.
For the following tips, only feed without a veterinary visit if your rabbit is licking and swallowing voluntarily and if you are confident there are no other health issues that may contraindicate the medications:
- Metacam (Meloxicam) can be given for pain 0.3-0.6 mg/kg once or twice a day and up to 1.5mg/kg without accumulation. This is generally at least 0.1cc per lb. Make sure your rabbit is hydrated and not showing signs of anemia when giving NSAIDs. Dosage calculator: https://www.vgr1.com/metacam/calc1/
- If your rabbit has not eaten in over 8 hours and shows no signs of bloating, assist feed 10-20cc (1-2 Tbsp) of Critical Care, pellet mash, or pumpkin puree to make sure there is food and fiber in their system for calories and to encourage digestive movement. If you are unsure if your rabbit is bloated, it is best to avoid adding more food in the stomach and find your closest veterinary clinic as soon as possible. Syringe feeding with a bloated stomach can make the issue worse and rupture their stomach from the pressure.
- A gut motility drug such as cisapride (Propulsid) or metoclopramide (Reglan) can be given to help get your rabbit's GI tract working again only if there is no blockage. The dosage is 0.1cc per pound of body weight.[7] You may also use ranitidine (Zantac), an over-the-counter drug, as a pro-kinetic in an emergency at a dosage of 2-5 mg/kg orally.[8] It also has anti-ulcerative qualities and useful in stressed rabbits.[9]
For ranitidine, you can crush either one 75mg tablet in 3.3cc of water OR one 150mg tablet in 6.6cc of water. 0.1cc should be given per pound every 12 hours or every 8 hours if dire. The solution can be stored for up to a week.
In September 2019, the carcinogen N-nitrosodimethylamine (NDMA) was found in some ranitidine products. As of April 2020, the FDA has requested the removal of all products containing ranitidine, both tablet and liquid.[10] The EU and Australia has also suspended usage and distribution of the medicine. If using ranitidine for your rabbit, please proceed with caution.
Extra resources
- Kinenchen. Is my bunny sick?
- Ethos Veterinary Health. (2020). Gastric Stasis: When to Refer and When to Send Them Home
- UNSW Sydney - Research Ethics & Compliance Support. (2020). Guidelines for the Management of Gastrointestinal Stasis in Rabbits [PDF]
- Jo Hinde and Molly Varga. (2019). Working together on gut stasis
- Molly Varga BVetMed DZooMed, MRCVS. (2016). Medical support of gut function in rabbits [PDF]
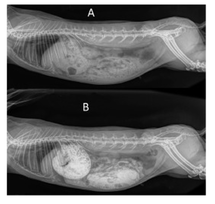
X-rays
Problems
"Rabbit intestines have been noted to be difficult to visualize in radiographs due to thin walls and surrounding structures obscuring edges. A recent study determined the dose of an iodine containing radio-opaque contrast agent, diatrizoate, and timings of radiographs to better visualise passage though the intestine and improved visualization of the gastrointestinal system. It was found the 7 ml/kg PO dose achieved contrast media in the ceceum after 45 mins. For more information about this study, please read the recent volume of Journal of Exotic Pet Medicine." - Association of Exotic Mammal Veterinarians
Dierig, J., Fehr, M., Eckert, Y., Hetterich,J., Thole, M., Rohn,K.,Reuschel, M. 2021. Diatrizoate contrast agent study for luminal patency and visualisation of the gastrointestinal tract in healthy rabbits (Oryctolagus cuniculus) and its influence on selected blood parameters and fecal quality. Journal of Exotic Pet Medicine. 37.8-15.
Further reading
- Cathy Emery. (2021). Cathy’s Critter Corner: A common rabbit condition for review — Exploring GI stasis
- Barbara L. Oglesbee, DVM, et al. (2020). Gastrointestinal Diseases of Rabbits (Graphic)
- Inquisitive Vet. (2020). Gastrointestinal Stasis in the Rabbit
- Long Beach Animal Hospital. (2020). GI Stasis (hairballs) in Rabbits (Graphic)
- Minh Huynh et al. (2014). Retrospective cohort study of gastrointestinal stasis in pet rabbits [PDF]
- Jennifer Prebble. (2012). Gastrointestinal stasis and obstructive Ileus in the rabbit
- Dana Krempels, Ph.D. (2005). GastroIntestinal Stasis, The Silent Killer
- Dana Krempels, Ph.D. et al. (2000). Ileus in domestic rabbits [PDF]
- Dana Krempels, Ph.D. (1996). Detecting Illness Before it's an Emergency
See also
- Acute gastrointestinal dilation
- Anorexia
- Cachexia
- Digestive system
- Hepatic lipidosis
- Liver lobe torsion
- Rabbit poop
- Veterinary emergencies
References
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 1.12 1.13 1.14 1.15 1.16 1.17 1.18 Varga, M. (2013). Textbook of rabbit medicine. (2nd ed.).
- ↑ Ethos Veterinary Health. (2020). Gastric Stasis in Rabbits. Retrieved 09 Mar 2023 from https://www.ethosvet.com/blog-post/gastric-stasis-when-to-refer-and-when-to-send-them-home/
- ↑ 3.00 3.01 3.02 3.03 3.04 3.05 3.06 3.07 3.08 3.09 3.10 Quesenberry, K & Carpenter, J. (2012). Ferrets, rabbits, and rodents: Clinical medicine and surgery. (3rd ed.).
- ↑ Sarah M Ozawa et al. (2019). Pharmacokinetics of maropitant citrate in New Zealand White rabbits ( Oryctolagus cuniculus). Retrieved 11 May 2023 from https://pubmed.ncbi.nlm.nih.gov/31556710/
- ↑ Kimberly M Oparil et al. (2019). Clinical characteristics and short-term outcomes for rabbits with signs of gastrointestinal tract dysfunction: 117 cases (2014-2016). Retrieved 27 Feb 2023 from https://www.researchgate.net/publication/336181390_Clinical_characteristics_and_short-term_outcomes_for_rabbits_with_signs_of_gastrointestinal_tract_dysfunction_117_cases_2014-2016
- ↑ 6.0 6.1 6.2 6.3 Krempels, D. (2005). GastroIntestinal Stasis, The Silent Killer. Retrieved 8 Mar 2016 from http://www.bio.miami.edu/hare/ileus.html
- ↑ House Rabbit Society MD, DC, & NoVA. (n.d.). Help Me Make It Through the Night. Retrieved 18 Sep 2020 from http://rabbitsinthehouse.org/newsletter/HRS-HelpMeMakeIt.pdf
- ↑ Carpenter, J. (2010). Diagnosing and treating gastric ileus/stasis in rabbits (Proceedings). Retrieved 25 Feb 2019 from http://veterinarycalendar.dvm360.com/diagnosing-and-treating-gastric-ileusstasis-rabbits-proceedings?id=&sk=&date=&pageID=2
- ↑ Saunders, R; Clark, M. (2012). Managing GI stasis in rabbits. Retrieved 25 Feb 2019 from https://www.vettimes.co.uk/article/managing-gi-stasis-in-rabbits/?format=pdf
- ↑ U.S. Food and Drug Administration (2020). FDA Requests Removal of all Ranitidine (Zantac) Products from the Market. Retrieved 22 Sep 2020 from https://www.fda.gov/news-events/press-announcements/fda-requests-removal-all-ranitidine-products-zantac-market